Module 1: Public Health Planning

What is Planning Fundamentals?
Planning Fundamentals is a self-directed, online course created by the Diabetes Training and Technical Assistance Center (DTTAC) at Emory University with support from the Centers for Disease Control and Prevention’s Division of Diabetes Translation. The curriculum content was developed in collaboration with M. Jean Gearing, MA, PhD, MPH and Pat Schumacher, MS, RD, Program and Evaluation Branch, Division of Diabetes Translation, with input from state department of health staff.
Planning Fundamentals provides
- a comprehensive overview of a process for developing and implementing a state plan for diabetes or for chronic disease prevention and control (referred to throughout the course as a ‘state plan’)
- video vignettes of state department of health staff and their partners demonstrating real world practice to encourage reflection on course learning
- downloadable resources to help guide the step-by-step planning process
Planning Fundamentals contains eight sequenced modules. Each module can be completed:
- in a group or individually
- at your own pace
- from any location
Who should take the Planning Fundamentals course?
The course is designed for state department of health staff and their partners who are working collaboratively to develop diabetes or chronic disease state plans. While some of the examples, video vignettes and resources in the course are specific to the world of diabetes prevention and control, the content of the course is applicable across chronic disease program areas.
Module 1: Introducing Planning from a Public Health Perspective
Module 1 provides an overview of the foundational knowledge needed to begin the public health planning process, with the goal of creating and implementing a state plan.
Creating a state plan is a lot like planting a garden – to be successful you need to have the right tools, an understanding of the weather and soil conditions in your area, and seeds that will grow well in those conditions. To follow this analogy, each Planning Fundamentals module is matched with different stages of the gardening process. Module 1 is similar to learning the basics of gardening.
Module Title |
Topics Covered |
Gardening Analogy |
|---|---|---|
Module 1: |
An Introduction to Public Health Planning |
|
Module 1 Learning Objectives:
Upon completion of this module, you should be able to:
- Explain the public health approach to addressing population health problems.
- Describe key concepts in the public health planning process.
Time estimate for completion:
It should take approximately 30 minutes to complete this module.
Section I: Public Health Planning
Introduction to the Public Health Approach
Public Health is the science of protecting and improving the health of entire populations through education, promotion of healthy lifestyles, and other preventive efforts. To be successful, these efforts require the analysis of public health problems and careful planning of interventions that address them.
Public health planning is a process that addresses the burden of disease by bringing together a wide array of partners across multiple sectors. The partners review epidemiological data and research about solutions to the burden of disease and use this information to set priorities and then plan and implement interventions to reduce the burden of disease. Using this approach to develop your state plan will help your plan flourish like a well-tended garden. You, like the master gardener, will have the tools and will follow the steps to create a rewarding end result.
Section I: Public Health Planning cont'd
The Public Health Approach to Addressing Health Problems
The core concept behind the public health approach is the scientific method. The scientific method states that observations of relationships between phenomenon, including the causes and cures for disease, must be tested, and that facts must collected and analyzed before moving forward with actions based on hypotheses about risk and prevention. The public health approach restates the scientific method in public health terms.
The Public Health Approach to addressing health problems in populations includes the following steps:
- Defining the problem and risk and preventive factors, using surveillance, epidemiologic, pathophysiologic, and other data
- Finding out what works to prevent and control the disease/injury through primary research and review of scientific literature
- Disseminating and scaling up effective interventions in a wide range of settings
- Monitoring and evaluating the impact and cost-effectiveness of these interventions
Section I: Public Health Planning cont'd
Defining a Public Health Problem
The public health approach is used to address public health problems. A disease, condition, or type of injury is considered a public health problem when:
- It has serious consequences for individuals affected, including high rates of morbidity, disability, and premature death
- It affects a significant proportion of the population
- Treatment of the disease/injury contributes significantly to health care costs and lost productivity
- Risk and preventive factors are known and understood
- The disease/injury is preventable
- Effective, early treatment reduces complications and costs
Section I: Public Health Planning cont'd
Defining Chronic Disease
A chronic disease is a disease for which there is no cure – once affected, an individual must live with the disease for the rest of his or her life. Most chronic diseases are progressive in their effects. The longer an individual has the disease, the higher the risk for complications and premature mortality.
The treatment of chronic diseases focuses on alleviating symptoms, slowing the progression of the disease, and educating the patient about self-management, or the adoption of healthy behaviors.
Section I: Public Health Planning cont'd
Diabetes as a Public Health Problem
Diabetes is an example of a chronic disease that meets all of the criteria for being a public health problem. Diabetes by the numbers:
- Thought Provoker: What makes diabetes a public health problem, based on the criteria presented in this module?25.8 million people in the United States have diabetes - that’s 8.3% of the total population
- 7.0 million of those cases are undiagnosed
- Diabetes cost the U.S. economy $174 billion in 2007
- Diabetes is the 7th leading cause of death in the U.S.
- One in three U.S. adults will have diabetes by the year 2050 if current trends continue
Click here for the 2011 National Diabetes Fact Sheet.
While these numbers are sobering, this outlook can be improved by using the public health approach and focusing on population-level change.
Section I: Public Health Planning cont'd
Population Health and Health Promotion
While public health has roots in communicable disease prevention and sanitation, over time, the mission of public health has grown to include protecting and improving the health of populations in other ways. Population health expanded the biomedical model of disease from causative agents and individual physiological response to include social factors as contributors to disease. One agent alone does not create health or disease, and health care delivery alone does not prevent a disease.
Public health programs focus on the prevention of chronic disease and the promotion of healthy lifestyles through:
- Policy and Environmental Changes that establish conditions where the healthy choice is the default choice
- Systems Changes in which social institutions or sectors implement widespread changes that encompass policy and environmental change
- Behavior Changes influenced by increased awareness of risk and protective behaviors and changed perceptions and beliefs about these behaviors due to health promotion, social marketing, and health communication efforts
Section I: Public Health Planning cont'd
The Socio-Ecological Model
The recognition that social and environmental conditions influence health has become known as the social determinants of health (SDOH) approach. The model that emerged in public health linking all of the different levels of influence on health and disease became known as the Socio-Ecological Model. The model demonstrates how health and disease are the result of multiple factors operating at multiple levels of social life, from the physical environment down to individual behavior. All of the levels are interconnected and change in one level can affect the others. While several versions of the socio-ecological model exist, the conceptualization of the model below will be used later in this course when describing a process for selecting linked interventions that target multiple levels.
Hover over each level for more details
Hover your mouse over each level for more details.Section I: Public Health Planning cont'd
The Social Determinants of Health and Coalitions
Public health’s increased emphasis on the importance of the social determinants of health led to efforts to involve multiple partners inside and outside of the health care system in finding solutions. The use of collaborative, participatory methods to engage partners, especially through coalitions, began with public health planning at the community level. Tools such as MAPP (Mobilizing for Action through Planning and Partnerships) and the Community Toolbox emerged to guide community coalitions through collaborative, participatory methods to apply the public health approach to addressing health problems.
Section I: Public Health Planning cont'd
The Health Impact Pyramid
There is a current emphasis in public health on “winnable battles” – or focusing resources strategically to achieve measureable impact on critical public health issues in a short amount of time. The criteria for these “winnable battles” echo the steps of the public health approach. Winnable battle strategies:
- Are evidence-based and feasible
- Have a significant impact on health
- Reach a high proportion of those at risk
- Have measureable impact
The effectiveness of different public health strategies is demonstrated through the five-tier Health Impact Pyramid, shown below. In this diagram, the degree of impact on population health determines the place of interventions on the pyramid. Interventions with the greatest impact are at the base of the pyramid, and interventions of lesser impact are at the top. Interventions focusing on lower levels of the pyramid, such as policy, environment, or social norm change, tend to be more effective because they reach broader segments of society and require less individual effort. Interventions at the top, such as those that educate and counsel individual patients, are less effective at the population level, but are still a necessary component of comprehensive public health strategies.
Health Impact Pyramid Diagram
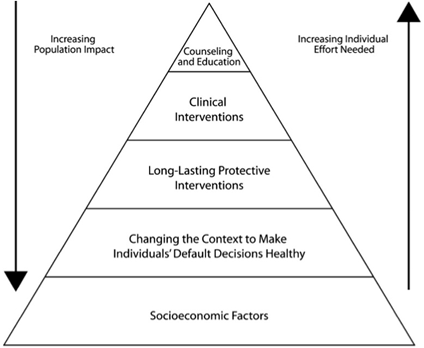
The most effective public health strategies are comprehensive and implement measures at each level. In order to accomplish this, a wide range of partners representing agencies, organizations, and communities that influence health in your state will need to be a part of the planning process.
Section Summary
Section 1 Summary
Section I discussed the public health approach to population-level health problems. The effects of the social and physical environment on these problems were described through:
- the Social Determinants of Health
- the Socio-Ecological Model
- the Health Impact Pyramid
The next section of Module 1 provides an overview of the public health planning process within the context of creating a state plan.
Section II: The Planning Process
Creating State Plans
be done to prevent and reduce the burden of diabetes or chronic disease in your state. It describes the proposed work of state department of health staff and the work of your partners.
When creating a state plan for diabetes or chronic disease prevention and control, the goal of the planning process is to develop, implement, and evaluate a multi-year statewide plan that uses evidence-based strategies and interventions to achieve measurable health impact.
A state plan for diabetes or chronic disease includes:
- Clear objectives and activities
- Explanation of the roles and responsibilities of partners and the state department of health
- Specific timelines
- Measures of success
The planning process creates a shared vision of the future of your state without the burden of diabetes or chronic disease and builds an understanding of what needs to be done to change the problem. The process of creating the state plan keeps your program focused and moving in a consistent direction.
Producing a state plan to address the burden of diabetes or other chronic diseases is an essential public health function. The next section reviews the key concepts in the planning process which were described previously. These concepts will be explored in more detail in modules 2 through 8.
Section II: The Planning Process cont'd
Planning is Inclusive and Engages Partners
Engaging partners from multiple sectors in assessment, planning, implementation, and evaluation of population health initiatives is critical to efforts to improve population health.
The process of developing and implementing your state plan should include representatives from your existing coalition as well as representatives from a wide range of stakeholder groups. Planning involves getting the buy-in and commitment of partners not just to the planning process but to the implementation of the plan in the following years.
The planning process creates a shared vision of the future of your state without the burden of diabetes or chronic disease and builds an understanding of what needs to be done to change the problem. As a part of the planning process, you and your partners will describe what will be changed, how it will be changed, who will be involved in making change happen, and how you will determine you have succeeded.
Part of the work undertaken during the planning process includes determining who has the expertise, the resources, and the willingness to accomplish change, and securing the commitment of those entities and their resources to implement effective strategies.
Section II: The Planning Process cont'd
Planning is a Data-Driven Process
A key component of the planning process is an in-depth review of the diabetes or chronic disease burden in your state. You will use many sources of existing data to describe the current situation regarding the burden as well as how that situation has changed over time. Part of the process of presenting and reviewing data is explaining their significance to non-public health participants.
Surveillance and census data are useful in prioritizing which populations should be targeted for interventions, based on the proportion of the burden of diabetes or chronic disease they represent.
Data about socioeconomic, political, geographic, educational, and cultural features of populations with diabetes or chronic disease in your state tells you about the context within which you can implement interventions, including obstacles you may encounter and resources you can access.Section II: The Planning Process cont'd
Planning Identifies Priorities, Opportunities, and Gaps
The planning process includes a comprehensive environmental scan or review of existing programs and services delivered by all of the organizations and agencies that comprise the diabetes or chronic disease health system in your state. The diabetes or chronic disease health system includes all those entities that are working to address the needs of persons along the continuum of those at risk for or with diabetes or chronic disease.
This environmental scan or program review should compare existing programs and services against the recommendations in the scientific literature to assure that effective and evidence-based strategies are in place. This review will identify areas that need better interventions or areas in which interventions are lacking.
Section II: The Planning Process cont'd
Planning Supports Strategies with Measurable Public Health Impact
Public health planning is focused on the goal of achieving measurable health impact, so the planning process should foster agreement to stay focused on implementing strategies proven to be effective. The planning process also examines how the implementation process and outcomes of interventions will be measured and results reported to inform the ongoing planning process. The planning process produces not just the overall state plan but also implementation and evaluation plans for the selected interventions.
Section II: The Planning Process cont'd
Planning Is an Ongoing Process
Planning activities are ongoing – a state plan is not a document to be produced to sit on a shelf or be posted on your website – it is a living charter that should guide you and your coalition’s work.
Planning is also an iterative process – feedback from the implementation (process evaluation) and results (outcome evaluation) should inform whether the course of action outlined in the state plan remains the same or is changed. Reviewing the plan and comparing actual activities and accomplishments to those you proposed in your plan should be the focus of at least one of your meetings with your coalition every year – and should be reviewed much more often by program staff. The plan is the template against which you and your partners can judge implementation and evaluation efforts.Section II: The Planning Process cont'd
Planning as a Management Tool
Finally, the planning process keeps your efforts to reduce the burden of diabetes or chronic disease focused and moving in a consistent direction. Your state plan serves as a template that allows you and your partners to measure progress and monitor performance. If desired outcomes are not achieved, you and your partners can modify interventions appropriately.
Section Summary
Section II Summary
Section II covered how public health planning is a:
- data-driven,
- inclusive; and
- ongoing process
During the process, priorities, opportunities, and gaps are identified and solutions that will result in measurable impact are selected and implemented.
Summary
Module 1 Summary
Module 1 introduced several concepts related to the public health approach, including population health, the socio-ecological model, and the social determinants of health. This module also explained the process of public health planning within the context of a creating a state plan.
Next, Modules 2-8 provide detailed information about the planning process, in the step-by-step order that you would follow when creating a state plan.
You can download a PDF of helpful resources for more information.
Congratulations, you have finished Module 1! Continue the course with Module 2: Coordinating the Planning Process.
 Module 4
Module 4 Module 7
Module 7