What is Diabetes?
Diabetes is a condition caused by an excessively high level of glucose in the blood.
To understand diabetes, we must first understand how the body processes food and converts it into the energy we need for daily activity. The food we eat is broken down into various components, one of them being glucose (sugar). Glucose is the substance that fuels the cells in the body. The blood transports glucose through the blood stream to cells throughout the body.
However, the cells do not automatically absorb glucose. They require insulin to unlock the cells and allow the glucose to enter and be converted into energy. Insulin is a hormone produced by beta cells in the pancreas, a large gland behind the stomach. If the pancreas produces insufficient quantities of insulin, or if the body cannot use insulin properly (a condition known as insulin resistance), then glucose does not enter the cells. It stays in the blood and causes high blood sugar.
What is Diabetes? cont'd
A person receives a diagnosis of diabetes when his or her blood glucose levels are above normal because of a lack of insulin, insufficient quantities of insulin, or insulin resistance. There is no cure for diabetes. Managing the disease to prevent adverse health effects requires lifestyle modifications and, in most cases, medication. When diabetes is not controlled properly, glucose remains in the blood and can damage vital organs.
Types of Diabetes
There are three main types of diabetes: type 1, type 2, and gestational.
Type 1 diabetes develops when the body’s immune system destroys its beta cells, rendering the pancreas unable to produce insulin. Since the body no longer produces insulin, people with type 1 diabetes must administer it directly through daily injections or an insulin pump. Type 1 diabetes accounts for 5% to 10% of diagnosed cases of diabetes. It develops primarily in children and young adults, although it can occur at any age.
Type 2 diabetes develops when the body does not use insulin properly. Type 2 diabetes is the most common form of diabetes, accounting for 90% to 95% of all diagnosed cases. It develops mostly in adults but can develop at any age and is increasingly developing in children and adolescents. Type 2 diabetes is highly associated with obesity.
Type 2 diabetes can often be prevented or delayed in at-risk populations through lifestyle modifications involving weight loss and regular physical activity. Preventing type 2 diabetes is the focus of the National Diabetes Prevention Program.
Gestational diabetes develops during pregnancy when certain hormones diminish a mother’s ability to use insulin (causing insulin resistance). Gestational diabetes usually goes away after the baby is born, but it increases the mother’s risk of eventually developing type 2 diabetes. If the diabetes does not go away after the delivery, the mother probably had undiagnosed type 2 diabetes during pregnancy rather than gestational diabetes.
Symptoms of Diabetes
The symptoms of diabetes vary. They range from mild to severe, and sometimes there are no symptoms at all. These are the most common symptoms:
- Increased thirst
- Increased hunger
- Fatigue
- Increased urination, especially at night
- Weight loss
- Blurred vision
- Sores or infections that do not heal or are slow to heal
Complications of Diabetes
 Diabetes is recognized as one of the leading causes of death and disability in the United States.
Diabetes is recognized as one of the leading causes of death and disability in the United States.
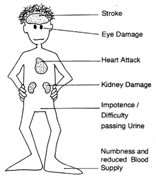
Over time, people with chronically high levels of blood glucose – a condition called hyperglycemia – suffer damage to their nerves and blood vessels. As a result, diabetes is linked to long-term complications that affect almost every part of the body.
Overall, the risk for premature death among people with diabetes is about twice the risk among people without diabetes.
CDC, National Diabetes Fact Sheet, 2011
Complications of Diabetes cont’d
The following are some of the possible complications of diabetes.
Hover your mouse over each complication for details:
Costs of Diabetes
 As a result of the many complications associated with the disease, diabetes exacts a considerable fiscal toll. The latest estimates place the national cost of diabetes at $176 billion a year. When the additional costs of undiagnosed diabetes, prediabetes, and gestational diabetes are factored in, the estimated figure rises to $245 billion (CDC, 2012).
As a result of the many complications associated with the disease, diabetes exacts a considerable fiscal toll. The latest estimates place the national cost of diabetes at $176 billion a year. When the additional costs of undiagnosed diabetes, prediabetes, and gestational diabetes are factored in, the estimated figure rises to $245 billion (CDC, 2012).
For a person with diagnosed diabetes, medical expenses can reach an average of nearly $12,000 a year, more than half of which is attributed to the disease.
Annual medical expenses for someone with diabetes are more than twice those of someone without diabetes (CDC, 2011)
Prevalence of Diabetes
 As reported in 2014 by CDC, the number of people in the United States with diabetes reached above 29 million, or 9.3% of the population.
As reported in 2014 by CDC, the number of people in the United States with diabetes reached above 29 million, or 9.3% of the population.
Of those 29 million people, 8.1 million (about 28%) do not know they have the disease.
Prevalence of Diabetes cont’d
 These data on diabetes in the United States become even more striking when broken down by group:
These data on diabetes in the United States become even more striking when broken down by group:
Prevalence of diabetes by age group:
- People aged 20 years or older: more than 1 in 10 (12.3%)
- People aged 60 years or older: more than 1 in 4 (25.9%)
Prevalence of Diabetes cont’d
Prevalence of diabetes by race or ethnicity (for adults aged 20 or older after adjusting for population age differences):
- 7.6% of non-Hispanic whites.
- 9.0% of Asian Americans.
- 12.8% of Hispanics.
- 13.2% of non-Hispanic blacks.
- 15.9% of American Indians and Alaska Natives.
Diabetes causes more deaths per year than breast cancer and AIDS combined.
American Diabetes Association
National Diabetes Data
This map shows the percentage of U.S. adults aged 20 or older with diagnosed diabetes (1994 to 2010).
 As you look at the maps, notice how the colors change across the country from light to dark. The darker the color, the higher the percentage of people with diagnosed diabetes. These maps depict how the percentage of adults with diagnosed diabetes increased from 1994 through 2010. These data include only adults, not children with diabetes, and account for only diagnosed cases. The actual number of people with the disease is higher because people with diabetes often do not know they have the disease until they experience symptoms or complications.
As you look at the maps, notice how the colors change across the country from light to dark. The darker the color, the higher the percentage of people with diagnosed diabetes. These maps depict how the percentage of adults with diagnosed diabetes increased from 1994 through 2010. These data include only adults, not children with diabetes, and account for only diagnosed cases. The actual number of people with the disease is higher because people with diabetes often do not know they have the disease until they experience symptoms or complications.
Furthermore, diabetes as an epidemic does not appear to be slowing. If current trends continue, CDC projects that one in three people born in 2000 will eventually develop diabetes.
What Is Behind the Diabetes Epidemic?
It is no coincidence that the increase in type 2 diabetes in the United States is mirrored by an increase in the number of people who are overweight or obese (80% to 90% of people with type 2 diabetes are overweight or obese). The reason for this relationship between weight and diabetes is not fully understood. It may be that cellular structure changes when people gain excess weight, making the cells less effective at using glucose.
Although the relationship between weight and type 2 diabetes is not fully understood, one undeniable finding is that maintained weight loss lowers risk for type 2 diabetes and makes it easier to manage the disease after it develops.
In the words of David Marrero, PhD,J.O., Indiana University School of Medicine:
 Type 2 diabetes usually does not stop people from continuing their lives as before. Its effects occur slowly and become more damaging over time as wear and tear on the body begins to affect many of the body’s systems. As an analogy, imagine that your car has been reliable for years – it is easy to drive around, goes as fast as you want it to, and has not had any major engine issues. Then you put 500 pounds of gravel in the trunk. At first it might just take your car a bit longer to get up to speed and require more gas to do so. Now imagine that the extra 500 pounds pinches your gas line so that even less gas gets from the tank to the engine. Now your car is really struggling to work.
Type 2 diabetes usually does not stop people from continuing their lives as before. Its effects occur slowly and become more damaging over time as wear and tear on the body begins to affect many of the body’s systems. As an analogy, imagine that your car has been reliable for years – it is easy to drive around, goes as fast as you want it to, and has not had any major engine issues. Then you put 500 pounds of gravel in the trunk. At first it might just take your car a bit longer to get up to speed and require more gas to do so. Now imagine that the extra 500 pounds pinches your gas line so that even less gas gets from the tank to the engine. Now your car is really struggling to work.
This analogy reflects what is happening in the body of someone who gains weight and does not get much physical activity. The extra weight is like the gravel in the trunk; the pancreas is forced to work harder to keep up with the body’s demands for energy. The body’s struggle for enough energy is compounded by lack of physical activity. As we become increasingly sedentary, insulin’s ability to access receptor sites (places in our bodies that take in insulin) is impaired (similar to pinching the fuel line). As a result, the body has a greater need to produce insulin but far less ability to use it effectively. In essence, the body’s “gas mileage” suffers. If one has too much weight and diminished receptor sites for insulin for a long enough time, the beta cells that make the insulin cannot keep pace. They become fatigued and eventually stop working properly. When this happens, type 2 diabetes develops.
Type 2 Diabetes and Obesity
Recall the previous U.S. map showing a dramatic increase in diabetes from 1994 through 2010. Now compare that map with this map showing the increase in obesity in the United States over roughly the same period (1994 to 2010).
In 1994, no state had an obesity rate higher than 19%. In 2010, only one state had a rate of 19% or less, and 68% of adults in the United States were overweight or obese.
Other Risk Factors for Type 2 Diabetes
In addition to overweight and obesity, numerous other factors are associated with risk for type 2 diabetes.
 Race and ethnicity
Race and ethnicity
Type 2 diabetes is most common among certain racial and ethnic groups.
- African Americans
- Hispanics
- American Indians and Alaska Natives
- Asian Americans
- Native Hawaiians and other Pacific islanders
Family history
Genetics play a role in diabetes risk. People with family members who have diabetes are at greater risk than are people without a family member with diabetes. The risk is especially high if the family member is a first degree relative (i.e., father, mother, sister, brother).
Risk Factors for Diabetes cont’d
 Lifestyle
Lifestyle
- Poor eating habits
- Engaging in a low level of physical activity
- Having low HDL cholesterol, high triglycerides, or high blood pressure
Age
Risk for type 2 diabetes increases with age: people older than 45 are at higher risk than are younger people. However the risk for type 2 diabetes is increasing for younger people.

Risk Factors for Diabetes cont’d
Gestational diabetes and large (macrosomic) babies
Women who had gestational diabetes, or who delivered a baby weighing 9 pounds or more, are at higher risk than women who did not have gestational diabetes. Women who had gestational diabetes have a 35% to 60% risk for diabetes in the following 10 to 20 years.
Prediabetes
With prediabetes the blood glucose level is higher than normal but not high enough to be diagnosed as type 2 diabetes. People with prediabetes show evidence of a metabolic defect, which is an early stage of insulin resistance.
Risk Factors for Diabetes cont’d
 Although many risk factors for diabetes are not modifiable, three are modifiable:
Although many risk factors for diabetes are not modifiable, three are modifiable:
- Weight
- Food choices
- Level of physical activity
Even overweight people with a family history of diabetes can decrease their risk for the disease by lowering their weight, improving their food choices, and increasing their level of physical activity. So, although type 2 diabetes is the most common form of diabetes, it is also preventable in many cases.
Maintained weight loss lowers the risk for type 2 diabetes.
Prediabetes
Prediabetes is a relatively new term. It is a condition in which a person’s blood glucose levels are higher than normal but not high enough for a diagnosis of type 2 diabetes. People with prediabetes have evidence of a metabolic defect that affects how they use insulin. This defect causes glucose to build up in their blood rather than be used by cells.
Without treatment (including lifestyle changes), people with prediabetes are at great risk for type 2 diabetes. They are also likely to experience adverse health conditions associated with diabetes, and they are at risk for cardiovascular disease.
The good news is that, with healthy lifestyle changes (including weight loss and increased physical activity), many people with prediabetes can restore their blood glucose to normal.
Prevalence of Prediabetes
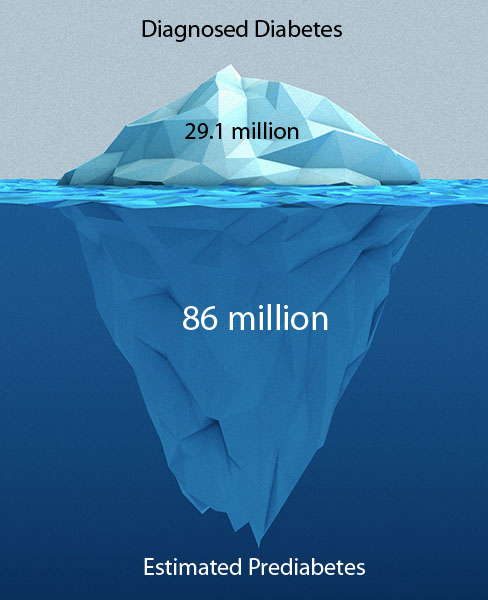 “Tip of the iceberg” is a common analogy for current levels of diabetes, and it is easy to see why. More than 29 million Americans have diabetes. However, CDC estimates that 86 million more have prediabetes (CDC, 2014). This means that about 27% of U.S. adults have prediabetes. Moreover, if the national rates of obesity remain high, this figure is likely to grow.
“Tip of the iceberg” is a common analogy for current levels of diabetes, and it is easy to see why. More than 29 million Americans have diabetes. However, CDC estimates that 86 million more have prediabetes (CDC, 2014). This means that about 27% of U.S. adults have prediabetes. Moreover, if the national rates of obesity remain high, this figure is likely to grow.
If left untreated, prediabetes progresses to diabetes at a rate of 5% to 15% per year. At current levels, this finding means an additional 4 to 12 million cases of diabetes a year.
Diagnostic Testing
Testing for diabetes and prediabetes should be done by a health care provider. Currently three tests can be administered:
Fasting plasma glucose (FPG) test - This test measures the level of impaired fasting glucose (IFG): a person’s blood glucose is measured in the morning after an 8-hour fast.
- Normal: 99 mg/dL (milligrams per deciliter) or lower
- Prediabetes: from 100 to 125 mg/dL
- Diabetes: 126 mg/dL or higher
Oral glucose tolerance test (OGTT) - This test measures for impaired glucose tolerance (IGT): a person’s blood glucose is measured after an 8-hour fast and again 2 hours after drinking a glucose-rich solution. A person with normal blood glucose has a predictable rise and fall in blood glucose level after drinking 75 grams of glucose. However, the blood glucose levels of a person with prediabetes or diabetes stay high for longer and are slow to go down after drinking the glucose solution.
- Normal: 139 mg/dL or lower
- Prediabetes: 140-199 mg/dL
- Diabetes: 200 mg/dL or higher
Diagnostic Testing contd
Glycated Hemoglobin (HbA1c) test - This test measures a person’s average blood glucose over 8 to 12 weeks before the test is administered. Fasting is not necessary.
- Normal: HbA1c lower than 5.7%
- Prediabetes: HbA1c 5.7% to 6.4%
- Diabetes: HbA1c higher than 6.4%
Note: The numbers indicating normal, prediabetes, or diabetes can change
from time to time as a result of new research findings.
Who Should be Tested for Prediabetes and Type 2 Diabetes?
People with either prediabetes or type 2 diabetes often do not experience any symptoms, yet it is important for people who meet certain criteria to have their blood glucose levels tested. The American Diabetes Association recommends that people who are overweight or obese and have one or more of the following additional risk factors should be tested for prediabetes and diabetes.
- Older than age of 45
- Physically inactive
- A parent, brother, or sister with diabetes
- African American, Alaska Native, American Indian, Asian American, Hispanic, or Pacific Islander
- Gave birth to a baby weighing 9 pounds or more or diagnosed gestational diabetes
- High blood pressure (140/90 mmHg or higher) or undergoing treatment for high blood pressure
- HDL (“good” cholesterol) lower than 35 mg/dL or a triglyceride level higher than 250 mg/dL
- Other conditions associated with insulin resistance (severe obesity, acanthosis nigricans).
- Impaired fasting glucose or impaired glucose tolerance
- Polycystic ovary syndrome
- History of cardiovascular disease
Rationale for Prevention
 The surging rates of diabetes are in no way limited to the United States. The incidence of diabetes is increasing in epidemic proportions throughout the world. According to a recent study, the number of obese people in the world has nearly doubled in the last 30 years (Finucane, 2011). Current estimates of prediabetes indicate that the scope of the disease is likely to get even worse – and soon – if sufficient prevention programs are not implemented.
The surging rates of diabetes are in no way limited to the United States. The incidence of diabetes is increasing in epidemic proportions throughout the world. According to a recent study, the number of obese people in the world has nearly doubled in the last 30 years (Finucane, 2011). Current estimates of prediabetes indicate that the scope of the disease is likely to get even worse – and soon – if sufficient prevention programs are not implemented.
The prevalence of type 2 diabetes increased rapidly during the past 20 years, becoming one of most devastating public health issues in the world today.
Rationale for Prevention cont’d
 Furthermore, diabetes is a disease that can be managed but not cured. However, managing the disease is challenging, and even the best treatment may not restore normal glucose levels or eliminate the risk for adverse complications.
Furthermore, diabetes is a disease that can be managed but not cured. However, managing the disease is challenging, and even the best treatment may not restore normal glucose levels or eliminate the risk for adverse complications.
Take Home Messages
- Diabetes is a condition characterized by higher than normal blood glucose levels due to insufficient quantities of insulin, insulin resistance, or both. Diabetes can cause many health-related complications.
- As of 2014, the number of people in the United States with diabetes reached more than 29 million, or 9.3% of the population. Of those people, 8 million (approximately 28%) do not know they have the disease.
- The number of new cases of type 2 diabetes is increasing in epidemic proportions throughout the world, and rates will continue to rise unless effective prevention programs are put in place and carried through.
- Obesity is a primary risk factor for type 2 diabetes. The rising rates of type 2 diabetes mirror the rising rates of overweight and obesity.
Take Home Messages cont'd
- Prediabetes is a condition in which blood glucose levels are high but not high enough to be type 2 diabetes. Having prediabetes can negatively affect one’s health and, if not treated, may progress to type 2 diabetes.
- According to recent reports from CDC, 86 million Americans have prediabetes (more than 1 out of 3 adults have prediabetes).
- Type 2 diabetes is preventable by structured lifestyle modification. Such modifications are the basis of the National Diabetes Prevention Program Lifestyle Intervention.